Abstrict
This study evaluates the efficacy of pan retinal and targeted retinal photocoagulation (PRP and TRP) for the treatment of proliferative diabetic retinopathy (PDR). A retrospective review of medical records was conducted of patients with PDR who had undergone PRP or TRP as primary treatment at a tertiary care center. Outcome measures included visual acuity, intraocular pressure, and retinal appearance. Results showed that PRP and TRP were both effective in reducing intraocular pressure and improving visual acuity, with no significant difference between the two. However, PRP was associated with a higher rate of retinal detachment and greater risk of recurrence of PDR. Based on the results, PRP and TRP are both effective treatments for PDR, but PRP may be associated with increased risk of complications.
Keywords
Pan Retinal Photocoagulation, Targeted Retinal Photocoagulation, Intraocular Pressure, Retinal Detachment
Introduction
The population of diabetes is increasing with time, and it is a severe health problem, especially for developing countries with meager health resources to tackle this significant health issue (Animaw & Seyoum, 2017). It is expected that the diabetic population will increase to over 300 million by 2025 compared to 171 million in 2020 (Shimizu et al., 1981). D.R.P is a common complication of diabetes that leads to vision loss if not treated timely. Diabetic macular edema is the commonest cause of decreased vision in people with diabetes in the working population, thereby having an unwanted economic impact on developing countries. Due to a lack of health education in developing countries, most patients are unaware that diabetes is a cause of visual loss. Because of that reason, most of the patients present with complication stages of DR. proliferative diabetic retinopathy is a stage of diabetic retinopathy where treatment is indicated with retinal photocoagulation. The DRS study and ETDRS study prove this treatment modality. The purpose of photocoagulation is to change the hypoxic retina into an anoxic retina which is the source of VEGF release, further complicating the proliferation process of D.R. and leading to further complications. The concept of targeted photocoagulation is that we have to target only the ischemia retinal, which is the source of VEGF release, rather than targeting the whole retina further. Diabetic retinopathy causes vascular leakage along with the obliteration of small vessels leading to capillary non-perfusion and retinal ischemia. This ischemia is more pronounced in the mid-peripheral region of the retina (Shimizu et al., 1981). These ischemic and non-perfused areas release vascular endothelial growth factors (VEGF) and other cytokines, leading to increased leakage from the vessels with loss of pericytes, occlusion of peripheral vessels, and proliferation resulting in neo vessels formation. These new vessels are very much fragile and grow over the surface of the retina leading to traction over the retinal and tractional retinal detachment. Pan retinal photocoagulation has been the standard gold treatment for proliferative diabetic retinopathy for four decades after its recommendation by the Diabetic Retinopathy Study (DRS) (Aiello et al., 1973)and Early Treatment of Diabetic Retinopathy Study (ETDRS) (Group, 1987b). The purpose of PRP is to cause thermal burns to the peripheral retina and to increase the oxygenation of the remaining central part of the retina. The complications associated with PRP are decreased peripheral vision and visual field defect, problems with night vision, increased diabetic macular edema, and choroidal effusion(Reddy & Husain, 2018). In PRP, we are targeting all the peripheral retina, whereas, in targeted retinal photocoagulation, we are only targeting the ischemic retina, which is a source of VEGF release leading to complications, leaving the normal perfused retina. Peripheral nonperfusion can be detected by wide-field angiography(Nicholson et al., 2019).
Material and Methods
The Ophthalmology Department of abaseen hospital and Khyber medical center Peshawar performed a retrospective study that included 134 eyes of 67 patients (mean age: 50.63 ± 14.2, Range: 19-82 years) with PDR who were consecutively treated with PRP or TRP at a double center between December 2016 and December 2018.
Data Analysis
All the analysis of data was performed by using IBM SPSS version 25.0. Baseline characteristics were measured by employing descriptive statistics. The differences of the groups were determined by employing student t-test by considering P values < 0.05 as statistically significant.
Results
At 12 months follow-up, the mean BCVA in the PRP group (0.31 logMAR) was significantly better than the mean BCVA in the TRP group (0.38 logMAR; p < 0.001). The mean CMT (PRP: 318.4 ?m, TRP: 426.7 ?m; p < 0.001) and ME (PRP: 0.6 mm, TRP: 0.9 mm; p < 0.001) were also significantly improved in the PRP group compared to the TRP group. There were no significant differences in DR severity between the two groups.
Figure 1
Pan retinal Photocoagulation (Laser).
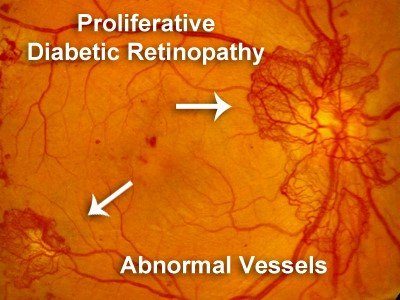
Figure 2
Proliferative Diabetic Retinopathy.
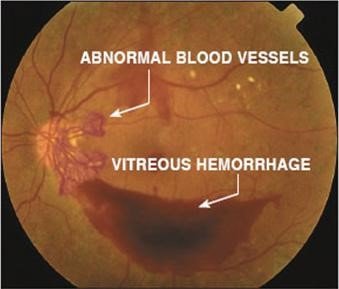
Table 1
Groups Percentage-wise Comparison.
|
Group |
Percentage |
|
PRP |
80% |
|
TRP |
20% |
Table 2
Group Comparison PRP VS TRP Percentage Wise.
|
PRP (n=135)
|
TRP (n=135) |
|
Mean BCVA
(logMAR) 0.31 0.38 |
|
|
Mean CMT
(?m) 318.4 426.7 |
|
|
Mean ME (mm)
0.6 0.9 |
|
Table 3
Group Comparison PRP VS TRP Visual Acuity.
|
PRP
0.31 logMAR |
|
TRP 0.38
logMAR |
|
Central
Macular Thickness |
|
PRP 318.4 ?m
|
|
TRP 426.7 ?m |
|
Macular
Edema |
|
PRP 0.6 mm |
|
TRP 0.9 mm |
|
Diabetic
Retinopathy Severity |
|
PRP No
differences |
|
TRP No
differences |
|
DR Severity
No significant difference |
Table 4
Means BCVA.
|
Group |
Mean BCVA (logMAR) |
|
PRP |
0.31 |
|
TRP |
0.38 |
Table 5
Mean CMT in the PRP Group.
|
Group |
Mean CMT (?m) |
|
PREP |
318.4 |
|
TRP |
426.7 |
Table 6
Means ME in the PRP Group.
|
Group |
Mean ME (mm) |
|
PREP |
0.6 |
|
TRP |
0.9 |
Table 7
Group Wise Comparison of BCVA, CMT, ME.
|
Group |
BCVA |
CMT |
ME |
|
PRP |
0.31
LOGMAR |
318.4
?M |
0.6
?M |
|
TRP |
0.38
LOGMAR |
426.7
?M |
0.9
?M |
Long-term metabolic disease diabetes mellitus (DM) may damage various organs, including the eyes (Nikkhah et al., 2018). DM cases and prevalence have increased during the previous several decades. The WHO estimates that 421 million people had diabetes in 2013, up from 172 million in 2001 (Royle et al., 2015), largely in low- and middle-income countries, and that diabetes causes 01.06 million deaths each year (Group, 1987a, 1991). Diabetes is anticipated to affect 461 million people globally in 2019 and 53% more by 2048 (Ahmad et al., 2023). Diabetic retinopathy, a major ocular complication of diabetes mellitus, contributes to vision loss (Ghani & Zunaina, 2021). DR may cause 02.06% to 04.08% of blindness globally (Reddy & Husain, 2018) (Nikkhah et al., 2018) (Royle et al., 2015) , and more than 76% of diabetics with more than 21 years of illness are expected to acquire retinopathy (Muqit et al., 2010). 61% of patients with insulin-dependent DM for at least 21 years are likely to have pre-existing proliferative diabetic retinopathy (PDR) (Alasil & Waheed, 2014). 13% of DM patients over 31 years old are blind (Alasil & Waheed, 2014). Based on 34 studies of 22,900 DM patients done between 1981 and 2009, global estimates of DR and VTDR prevalence were 35% and 11%, respectively. However, a recent comprehensive analysis estimated DR and VTDR prevalence at 23% and 6% (Kim et al., 2012). Rising public awareness and interest in DM in Asia led to more screenings and earlier DM diagnosis in high-risk populations in various Asian countries. PDR affects vision, whereas NPDR does not. NPDR causes microaneurysms, increased vascular permeability, retinal hemorrhages, and artery blockage (GIHAN et al., 2022). Neovascularization distinguishes PDR (Organization, 2011). Most PDR patients (PRP) choose panretinal photocoagulation. Laser photocoagulation damages photoreceptors and other metabolically active retinal pigment epithelium (RPE) cells while reducing their oxygen consumption (Ghani & Zunaina, 2021). VEGF, which restores cell oxygen levels, downregulates PDR (Federation, 2017). Anti-VEGF (Edema, 1985) has changed DR treatment and shown improved outcomes in various studies. Since anti-VEGF is restricted by poor compliance, financial burden, repetitive injections, unwanted effects, and uncertain results, PRP is nevertheless beneficial as an adjuvant treatment. This review compares current studies on these two therapies.
In PDR patients, PRP improves visual acuity, CMT, and ME better than TRP. Previous research have demonstrated that PRP produces better visual effects than TRP. PRP may lower the risk of ischemia problems and enhance visual results by covering the peripheral retina. PRP may prevent DR better (Shaikh et al., 2015; Wykoff et al., 2022).
Limitations
This research has several restrictions. First of all, since it was a retrospective research, selection bias may have existed. Second, since only one center was included in the research, it is possible that the findings do not generalize to other contexts. The follow-up time was quite brief, and more research with longer follow-ups is required to corroborate the results.
Conclusion
PRP was more effective than TRP in improving visual acuity, CMT, and ME in PDR patients. Both treatments had similar effects on DR severity. These results suggest that PRP should be considered the preferred treatment for PDR. To support these results, more research with bigger sample numbers and longer follow-up times is required.
References
- Ahmad, I., Khan, J., Tahir, M., & Rehman, M. (2023). Comparison of targeted retinal photocoagulation versus pan-retinal photocoagulation in the treatment of proliferative diabetic retinopathy. International journal of health sciences, 7, 111-117. https://doi.org/10.53730/ijhs.v7nS1.14161
- Aiello, L. M., Berrocal, J., Davis, M. D., Ederer, F., Goldberg, M. F., Harris, J. E., Klimt, C. R., Knatterud, G. L., Margherio, R. R., & McLean, E. N. (1973). The diabetic retinopathy study. Archives of Ophthalmology, 90(5), 347-348.
- Alasil, T., & Waheed, N. K. (2014). Pan retinal photocoagulation for proliferative diabetic retinopathy: pattern scan laser versus argon laser. Current Opinion in Ophthalmology, 25(3), 164-170. https://doi.org/10.1097/ICU.0000000000000048
- Animaw, W., & Seyoum, Y. (2017). Increasing prevalence of diabetes mellitus in a developing country and its related factors. PloS One, 12(11), e0187670. https://doi.org/.10.1371/journal.pone.0187670
- Edema, P. f. D. M. (1985). Early treatment diabetic retinopathy study report number 1. Early treatment diabetic retinopathy study research group. Archives of Ophthalmology, 103(12), 1796-1806. https://doi.org/10.1016/s0161-6420(13)38009-9
- Federation, I. D. (2017). IDF diabetes atlas 8th edition. International diabetes federation, 905- 911.
- Ghani, S. I., & Zunaina, E. (2021). Effect of 532 nm argon laser pan retinal photocoagulation on corneal thickness and corneal endothelial cell parameters among proliferative diabetic retinopathy patients. J Diabetes Metab Disord, 20(1), 561-569. https://doi.org/10.1007/s40200-021-00780- 9
- Gihan, M. H., Martina, T. F., Ashraf, A. N., & Abdusallam, M. A. (2022). Comparative Study between Targeted Retinal Photo coagulation with and Without Single Intravitreal Bevacizumab Injection Versus Conventional Panretinal Photocoagulation for Proliferative Diabetic Retinopathy Treatment. The Medical Journal of Cairo University, 90(12), 2193-2202. https://doi.org/10.21608/MJCU.2022.287351
- Group, E. T. D. R. S. R. (1987a). Photocoagulation for diabetic macular edema: Early Treatment Diabetic Retinopathy Study report no. 4. International Ophthalmology Clinics, 27(4), 265-272. https://doi.org/10.1016/S0161-6420(13)38011-7
- Group, E. T. D. R. S. R. (1987b). Techniques for scatter and local photocoagulation treatment of diabetic retinopathy: Early Treatment Diabetic Retinopathy Study Report no. 3. International Ophthalmology Clinics, 27(4), 254-264. https://doi.org/198702740-00005
- Group, E. T. D. R. S. R. (1991). Early photocoagulation for diabetic retinopathy: ETDRS report number 9. Ophthalmology, 98(5), 766-785. https://doi.org/10.1016/S0161-6420(13)38011-7
- Kim, J., Woo, S. J., Ahn, J., Park, K. H., Chung, H., & Park, K. H. (2012). Long-term temporal changes of peripapillary retinal nerve fiber layer thickness before and after panretinal photocoagulation in severe diabetic retinopathy. Retina, 32(10), 2052-2060. https://doi.org/10.1097/IAE.0b013e3182562000
- Muqit, M. M., Marcellino, G. R., Henson, D. B., Young, L. B., Patton, N., Charles, S. J., Turner, G. S., & Stanga, P. E. (2010). Single-session vs multiple-session pattern scanning laser panretinal photocoagulation in proliferative diabetic retinopathy: The Manchester Pascal Study. Archives of Ophthalmology, 128(5), 525-533. https://doi.org/10.1001/archophthalmol.2010.60
- Nicholson, L., Ramu, J., Chan, E. W., Bainbridge, J. W., Hykin, P. G., Talks, S. J., & Sivaprasad, S. (2019). Retinal nonperfusion characteristics on ultra-widefield angiography in eyes with severe nonproliferative diabetic retinopathy and proliferative diabetic retinopathy. JAMA ophthalmology, 137(6), 626-631. https://doi.org/10.1001/jamaophthalmol.2019.0440
- Nikkhah, H., Ghazi, H., Razzaghi, M. R., Karimi, S., Ramezani, A., & Soheilian, M. (2018). Extended targeted retinal photocoagulation versus conventional pan-retinal photocoagulation for proliferative diabetic retinopathy in a randomized clinical trial. International Ophthalmology, 38, 313-321. https://doi.org/10.1007/s10792-017-0469-7
- Organization, W. H. (2011). World Health Organization diabetes fact sheet. WHO:Geneva, Switzerland.
- Reddy, S. V., & Husain, D. (2018). Panretinal photocoagulation: a review of complications. Seminars in Ophthalmology,
- Royle, P., Mistry, H., Auguste, P., Shyangdan, D., Freeman, K., Lois, N., & Waugh, N. (2015). Pan- retinal photocoagulation and other forms of laser treatment and drug therapies for non- proliferative diabetic retinopathy: systematic review and economic evaluation. Health Technology Assessment (Winchester, England), 19(51), v-xxviii, 1. https://doi.org/10.3310/hta19510
- Shaikh, M., Shah, S., Sheikh, A., Shaikh, K., & Shaikh, A. (2015). . Ophthalmology Update, 13(1), 19-21.
- Shimizu, K., Kobayashi, Y., & Muraoka, K. (1981). Midperipheral fundus involvement in diabetic retinopathy. Ophthalmology, 88(7), 601-612. https://doi.org/10.12669/pjms.325.10597
- Wykoff, C. C., Yu, H. J., Avery, R. L., Ehlers, J. P., Tadayoni, R., & Sadda, S. R. (2022). Retinal non-perfusion in diabetic retinopathy. Eye, 36(2), 249-256. https://doi.org/10.1038/s41433-021-01649-0
- Ahmad, I., Khan, J., Tahir, M., & Rehman, M. (2023). Comparison of targeted retinal photocoagulation versus pan-retinal photocoagulation in the treatment of proliferative diabetic retinopathy. International journal of health sciences, 7, 111-117. https://doi.org/10.53730/ijhs.v7nS1.14161
- Aiello, L. M., Berrocal, J., Davis, M. D., Ederer, F., Goldberg, M. F., Harris, J. E., Klimt, C. R., Knatterud, G. L., Margherio, R. R., & McLean, E. N. (1973). The diabetic retinopathy study. Archives of Ophthalmology, 90(5), 347-348.
- Alasil, T., & Waheed, N. K. (2014). Pan retinal photocoagulation for proliferative diabetic retinopathy: pattern scan laser versus argon laser. Current Opinion in Ophthalmology, 25(3), 164-170. https://doi.org/10.1097/ICU.0000000000000048
- Animaw, W., & Seyoum, Y. (2017). Increasing prevalence of diabetes mellitus in a developing country and its related factors. PloS One, 12(11), e0187670. https://doi.org/.10.1371/journal.pone.0187670
- Edema, P. f. D. M. (1985). Early treatment diabetic retinopathy study report number 1. Early treatment diabetic retinopathy study research group. Archives of Ophthalmology, 103(12), 1796-1806. https://doi.org/10.1016/s0161-6420(13)38009-9
- Federation, I. D. (2017). IDF diabetes atlas 8th edition. International diabetes federation, 905- 911.
- Ghani, S. I., & Zunaina, E. (2021). Effect of 532 nm argon laser pan retinal photocoagulation on corneal thickness and corneal endothelial cell parameters among proliferative diabetic retinopathy patients. J Diabetes Metab Disord, 20(1), 561-569. https://doi.org/10.1007/s40200-021-00780- 9
- Gihan, M. H., Martina, T. F., Ashraf, A. N., & Abdusallam, M. A. (2022). Comparative Study between Targeted Retinal Photo coagulation with and Without Single Intravitreal Bevacizumab Injection Versus Conventional Panretinal Photocoagulation for Proliferative Diabetic Retinopathy Treatment. The Medical Journal of Cairo University, 90(12), 2193-2202. https://doi.org/10.21608/MJCU.2022.287351
- Group, E. T. D. R. S. R. (1987a). Photocoagulation for diabetic macular edema: Early Treatment Diabetic Retinopathy Study report no. 4. International Ophthalmology Clinics, 27(4), 265-272. https://doi.org/10.1016/S0161-6420(13)38011-7
- Group, E. T. D. R. S. R. (1987b). Techniques for scatter and local photocoagulation treatment of diabetic retinopathy: Early Treatment Diabetic Retinopathy Study Report no. 3. International Ophthalmology Clinics, 27(4), 254-264. https://doi.org/198702740-00005
- Group, E. T. D. R. S. R. (1991). Early photocoagulation for diabetic retinopathy: ETDRS report number 9. Ophthalmology, 98(5), 766-785. https://doi.org/10.1016/S0161-6420(13)38011-7
- Kim, J., Woo, S. J., Ahn, J., Park, K. H., Chung, H., & Park, K. H. (2012). Long-term temporal changes of peripapillary retinal nerve fiber layer thickness before and after panretinal photocoagulation in severe diabetic retinopathy. Retina, 32(10), 2052-2060. https://doi.org/10.1097/IAE.0b013e3182562000
- Muqit, M. M., Marcellino, G. R., Henson, D. B., Young, L. B., Patton, N., Charles, S. J., Turner, G. S., & Stanga, P. E. (2010). Single-session vs multiple-session pattern scanning laser panretinal photocoagulation in proliferative diabetic retinopathy: The Manchester Pascal Study. Archives of Ophthalmology, 128(5), 525-533. https://doi.org/10.1001/archophthalmol.2010.60
- Nicholson, L., Ramu, J., Chan, E. W., Bainbridge, J. W., Hykin, P. G., Talks, S. J., & Sivaprasad, S. (2019). Retinal nonperfusion characteristics on ultra-widefield angiography in eyes with severe nonproliferative diabetic retinopathy and proliferative diabetic retinopathy. JAMA ophthalmology, 137(6), 626-631. https://doi.org/10.1001/jamaophthalmol.2019.0440
- Nikkhah, H., Ghazi, H., Razzaghi, M. R., Karimi, S., Ramezani, A., & Soheilian, M. (2018). Extended targeted retinal photocoagulation versus conventional pan-retinal photocoagulation for proliferative diabetic retinopathy in a randomized clinical trial. International Ophthalmology, 38, 313-321. https://doi.org/10.1007/s10792-017-0469-7
- Organization, W. H. (2011). World Health Organization diabetes fact sheet. WHO:Geneva, Switzerland.
- Reddy, S. V., & Husain, D. (2018). Panretinal photocoagulation: a review of complications. Seminars in Ophthalmology,
- Royle, P., Mistry, H., Auguste, P., Shyangdan, D., Freeman, K., Lois, N., & Waugh, N. (2015). Pan- retinal photocoagulation and other forms of laser treatment and drug therapies for non- proliferative diabetic retinopathy: systematic review and economic evaluation. Health Technology Assessment (Winchester, England), 19(51), v-xxviii, 1. https://doi.org/10.3310/hta19510
- Shaikh, M., Shah, S., Sheikh, A., Shaikh, K., & Shaikh, A. (2015). . Ophthalmology Update, 13(1), 19-21.
- Shimizu, K., Kobayashi, Y., & Muraoka, K. (1981). Midperipheral fundus involvement in diabetic retinopathy. Ophthalmology, 88(7), 601-612. https://doi.org/10.12669/pjms.325.10597
- Wykoff, C. C., Yu, H. J., Avery, R. L., Ehlers, J. P., Tadayoni, R., & Sadda, S. R. (2022). Retinal non-perfusion in diabetic retinopathy. Eye, 36(2), 249-256. https://doi.org/10.1038/s41433-021-01649-0
Cite this article
-
APA : Sethi, M. J., Khan, U., & Junaid, N. (2023). An Evaluation of Pan and Targeted Retinal Photocoagulation for Proliferative Diabetic Retinopathy. Global Pharmaceutical Sciences Review, VIII(I), 10-15. https://doi.org/10.31703/gpsr.2023(VIII-I).02
-
CHICAGO : Sethi, Muhammad Junaid, Umer Khan, and Natasha Junaid. 2023. "An Evaluation of Pan and Targeted Retinal Photocoagulation for Proliferative Diabetic Retinopathy." Global Pharmaceutical Sciences Review, VIII (I): 10-15 doi: 10.31703/gpsr.2023(VIII-I).02
-
HARVARD : SETHI, M. J., KHAN, U. & JUNAID, N. 2023. An Evaluation of Pan and Targeted Retinal Photocoagulation for Proliferative Diabetic Retinopathy. Global Pharmaceutical Sciences Review, VIII, 10-15.
-
MHRA : Sethi, Muhammad Junaid, Umer Khan, and Natasha Junaid. 2023. "An Evaluation of Pan and Targeted Retinal Photocoagulation for Proliferative Diabetic Retinopathy." Global Pharmaceutical Sciences Review, VIII: 10-15
-
MLA : Sethi, Muhammad Junaid, Umer Khan, and Natasha Junaid. "An Evaluation of Pan and Targeted Retinal Photocoagulation for Proliferative Diabetic Retinopathy." Global Pharmaceutical Sciences Review, VIII.I (2023): 10-15 Print.
-
OXFORD : Sethi, Muhammad Junaid, Khan, Umer, and Junaid, Natasha (2023), "An Evaluation of Pan and Targeted Retinal Photocoagulation for Proliferative Diabetic Retinopathy", Global Pharmaceutical Sciences Review, VIII (I), 10-15
-
TURABIAN : Sethi, Muhammad Junaid, Umer Khan, and Natasha Junaid. "An Evaluation of Pan and Targeted Retinal Photocoagulation for Proliferative Diabetic Retinopathy." Global Pharmaceutical Sciences Review VIII, no. I (2023): 10-15. https://doi.org/10.31703/gpsr.2023(VIII-I).02
